Full text:
www.easternhealth.ca Page 1 of 4 DI-RAD-CP-006 v.1 (Oct11-18)
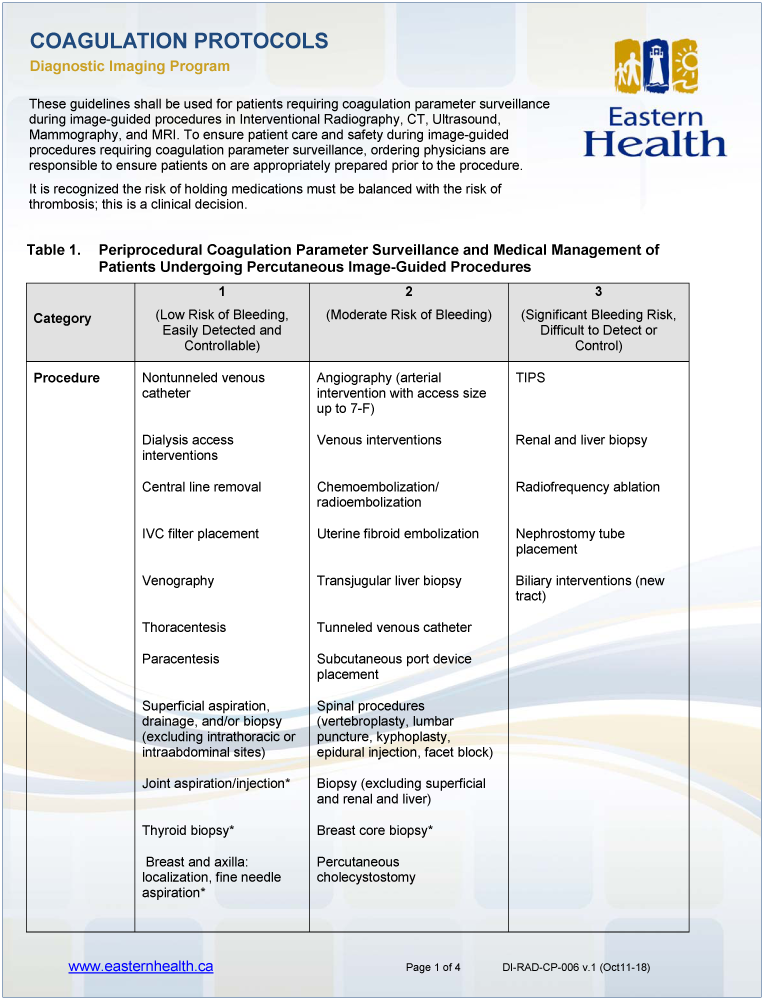
Table 1. Periprocedural Coagulation Parameter Surveillance and Medical Management of
Patients Undergoing Percutaneous Image-Guided Procedures
Category
1
(Low Risk of Bleeding,
Easily Detected and
Controllable)
2
(Moderate Risk of Bleeding)
3
(Significant Bleeding Risk,
Difficult to Detect or
Control)
Procedure Nontunneled venous
catheter
Angiography (arterial
intervention with access size
up to 7-F)
TIPS
Dialysis access
interventions
Venous interventions Renal and liver biopsy
Central line removal Chemoembolization/
radioembolization
Radiofrequency ablation
IVC filter placement Uterine fibroid embolization Nephrostomy tube
placement
Venography Transjugular liver biopsy Biliary interventions (new
tract)
Thoracentesis Tunneled venous catheter
Paracentesis Subcutaneous port device
placement
Superficial aspiration,
drainage, and/or biopsy
(excluding intrathoracic or
intraabdominal sites)
Spinal procedures
(vertebroplasty, lumbar
puncture, kyphoplasty,
epidural injection, facet block)
Joint aspiration/injection* Biopsy (excluding superficial
and renal and liver)
Thyroid biopsy* Breast core biopsy*
Breast and axilla:
localization, fine needle
aspiration*
Percutaneous
cholecystostomy
COAGULATION PROTOCOLS
Diagnostic Imaging Program
These guidelines shall be used for patients requiring coagulation parameter surveillance
during image-guided procedures in Interventional Radiography, CT, Ultrasound,
Mammography, and MRI. To ensure patient care and safety during image-guided
procedures requiring coagulation parameter surveillance, ordering physicians are
responsible to ensure patients on are appropriately prepared prior to the procedure.
It is recognized the risk of holding medications must be balanced with the risk of
thrombosis; this is a clinical decision.
www.easternhealth.ca Page 2 of 4 DI-RAD-CP-006 v.2 (Nov. 16-18)
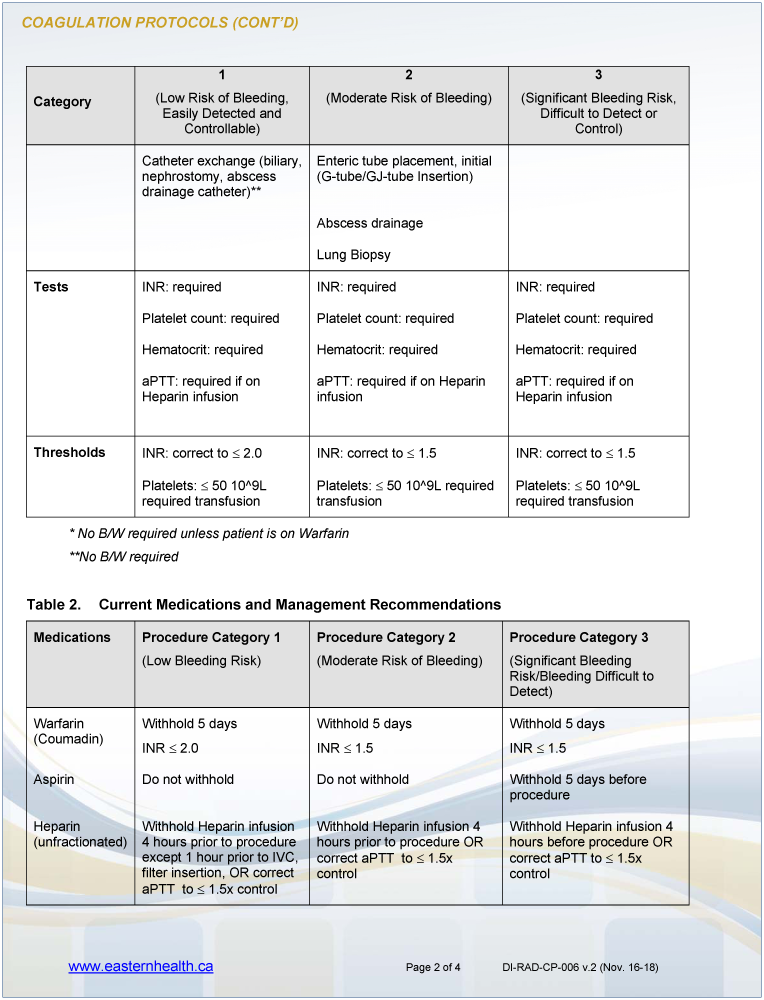
COAGULATION PROTOCOLS (CONT’D)
Category
1
(Low Risk of Bleeding,
Easily Detected and
Controllable)
2
(Moderate Risk of Bleeding)
3
(Significant Bleeding Risk,
Difficult to Detect or
Control)
Catheter exchange (biliary,
nephrostomy, abscess
drainage catheter)**
Enteric tube placement, initial
(G-tube/GJ-tube Insertion)
Abscess drainage
Lung Biopsy
Tests INR: required INR: required INR: required
Platelet count: required Platelet count: required Platelet count: required
Hematocrit: required Hematocrit: required Hematocrit: required
aPTT: required if on
Heparin infusion
aPTT: required if on Heparin
infusion
aPTT: required if on
Heparin infusion
Thresholds INR: correct to 2.0 INR: correct to 1.5 INR: correct to 1.5
Platelets: 50 10^9L
required transfusion
Platelets: 50 10^9L required
transfusion
Platelets: 50 10^9L
required transfusion
* No B/W required unless patient is on Warfarin
**No B/W required
Table 2. Current Medications and Management Recommendations
Medications Procedure Category 1
(Low Bleeding Risk)
Procedure Category 2
(Moderate Risk of Bleeding)
Procedure Category 3
(Significant Bleeding
Risk/Bleeding Difficult to
Detect)
Warfarin
(Coumadin)
Withhold 5 days
INR 2.0
Withhold 5 days
INR 1.5
Withhold 5 days
INR 1.5
Aspirin Do not withhold Do not withhold Withhold 5 days before
procedure
Heparin
(unfractionated)
Withhold Heparin infusion
4 hours prior to procedure
except 1 hour prior to IVC,
filter insertion, OR correct
aPTT to 1.5x control
Withhold Heparin infusion 4
hours prior to procedure OR
correct aPTT to 1.5x
control
Withhold Heparin infusion 4
hours before procedure OR
correct aPTT to 1.5x
control
www.easternhealth.ca Page 3 of 4 DI-RAD-CP-006 v.2 (Nov. 16-18)
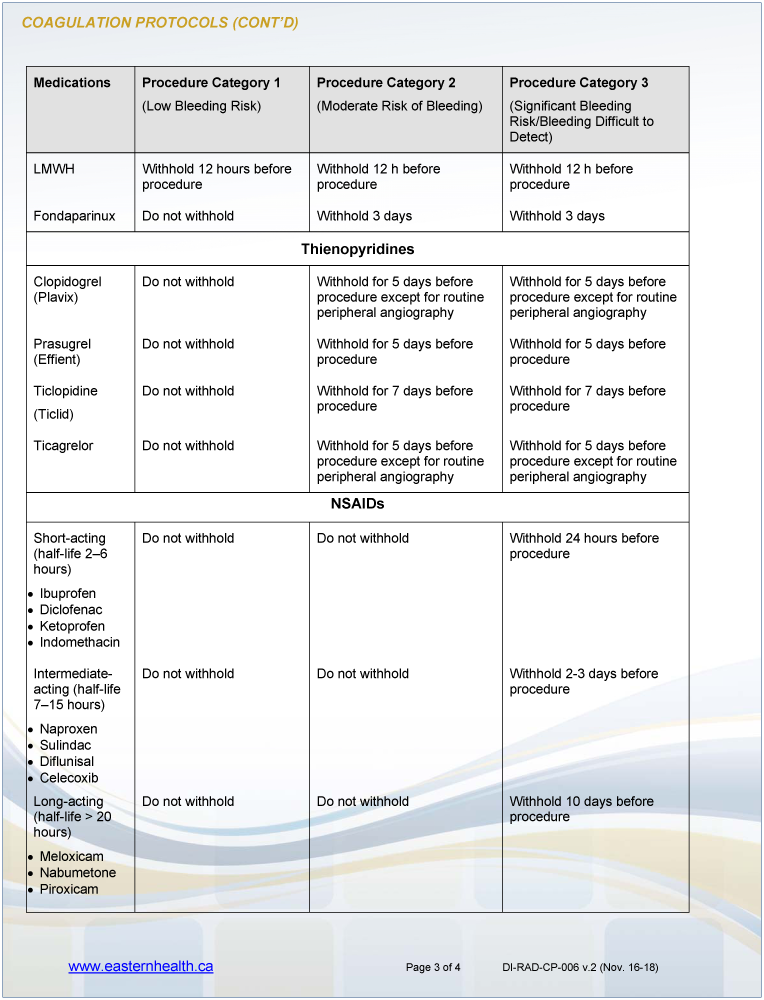
COAGULATION PROTOCOLS (CONT’D)
Medications Procedure Category 1
(Low Bleeding Risk)
Procedure Category 2
(Moderate Risk of Bleeding)
Procedure Category 3
(Significant Bleeding
Risk/Bleeding Difficult to
Detect)
LMWH Withhold 12 hours before
procedure
Withhold 12 h before
procedure
Withhold 12 h before
procedure
Fondaparinux Do not withhold Withhold 3 days Withhold 3 days
Thienopyridines
Clopidogrel
(Plavix)
Do not withhold Withhold for 5 days before
procedure except for routine
peripheral angiography
Withhold for 5 days before
procedure except for routine
peripheral angiography
Prasugrel
(Effient)
Do not withhold Withhold for 5 days before
procedure
Withhold for 5 days before
procedure
Ticlopidine
(Ticlid)
Do not withhold Withhold for 7 days before
procedure
Withhold for 7 days before
procedure
Ticagrelor Do not withhold Withhold for 5 days before
procedure except for routine
peripheral angiography
Withhold for 5 days before
procedure except for routine
peripheral angiography
NSAIDs
Short-acting
(half-life 2–6
hours)
Ibuprofen
Diclofenac
Ketoprofen
Indomethacin
Do not withhold Do not withhold Withhold 24 hours before
procedure
Intermediateacting
(half-life
7–15 hours)
Naproxen
Sulindac
Diflunisal
Celecoxib
Do not withhold Do not withhold Withhold 2-3 days before
procedure
Long-acting
(half-life > 20
hours)
Meloxicam
Nabumetone
Piroxicam
Do not withhold Do not withhold Withhold 10 days before
procedure
www.easternhealth.ca Page 4 of 4 DI-RAD-CP-006 v.2 (Nov. 16-18)
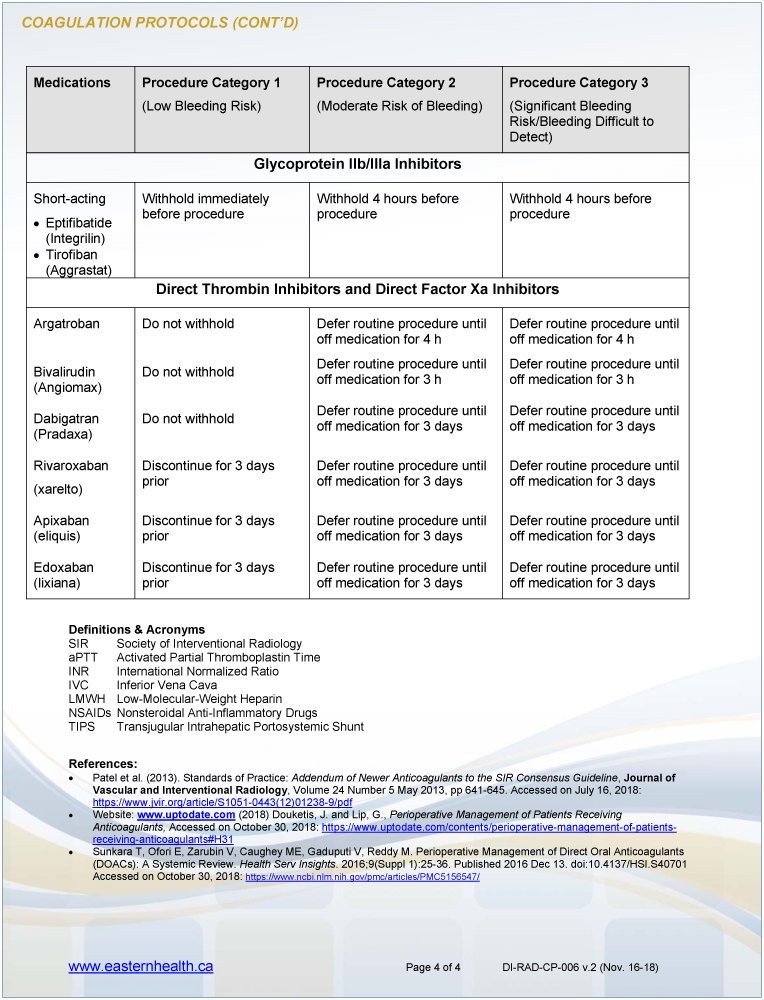
COAGULATION PROTOCOLS (CONT’D)
Medications Procedure Category 1
(Low Bleeding Risk)
Procedure Category 2
(Moderate Risk of Bleeding)
Procedure Category 3
(Significant Bleeding
Risk/Bleeding Difficult to
Detect)
Glycoprotein IIb/IIIa Inhibitors
Short-acting
Eptifibatide
(Integrilin)
Tirofiban
(Aggrastat)
Withhold immediately
before procedure
Withhold 4 hours before
procedure
Withhold 4 hours before
procedure
Direct Thrombin Inhibitors and Direct Factor Xa Inhibitors
Argatroban Do not withhold Defer routine procedure until
off medication for 4 h
Defer routine procedure until
off medication for 4 h
Bivalirudin
(Angiomax)
Do not withhold Defer routine procedure until
off medication for 3 h
Defer routine procedure until
off medication for 3 h
Dabigatran
(Pradaxa)
Do not withhold Defer routine procedure until
off medication for 3 days
Defer routine procedure until
off medication for 3 days
Rivaroxaban
(xarelto)
Discontinue for 3 days
prior
Defer routine procedure until
off medication for 3 days
Defer routine procedure until
off medication for 3 days
Apixaban
(eliquis)
Discontinue for 3 days
prior
Defer routine procedure until
off medication for 3 days
Defer routine procedure until
off medication for 3 days
Edoxaban
(lixiana)
Discontinue for 3 days
prior
Defer routine procedure until
off medication for 3 days
Defer routine procedure until
off medication for 3 days
Definitions & Acronyms
SIR Society of Interventional Radiology
aPTT Activated Partial Thromboplastin Time
INR International Normalized Ratio
IVC Inferior Vena Cava
LMWH Low-Molecular-Weight Heparin
NSAIDs Nonsteroidal Anti-Inflammatory Drugs
TIPS Transjugular Intrahepatic Portosystemic Shunt
References:
Patel et al. (2013). Standards of Practice: Addendum of Newer Anticoagulants to the SIR Consensus Guideline, Journal of
Vascular and Interventional Radiology, Volume 24 Number 5 May 2013, pp 641-645. Accessed on July 16, 2018:
https://www.jvir.org/article/S1051-0443(12)01238-9/pdf
Website: www.uptodate.com (2018) Douketis, J. and Lip, G., Perioperative Management of Patients Receiving
Anticoagulants, Accessed on October 30, 2018: https://www.uptodate.com/contents/perioperative-management-of-patientsreceiving-
anticoagulants#H31
Sunkara T, Ofori E, Zarubin V, Caughey ME, Gaduputi V, Reddy M. Perioperative Management of Direct Oral Anticoagulants
(DOACs): A Systemic Review. Health Serv Insights. 2016;9(Suppl 1):25-36. Published 2016 Dec 13. doi:10.4137/HSI.S40701
Accessed on October 30, 2018: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5156547/